Atopic dermatitis or eczema
Introduction
Atopic dermatitis (AD), often termed “eczema”, is a chronic pruritic skin condition that affects about 10-20% of children and about 2-3% of adults. It is characterized by extreme itching, dry skin, scaling, erythematous papules, excoriations and exudates. These symptoms may be associated with frequent skin infections, as well as an increased incidence of allergic rhinitis, food allergy, and asthma.
The clinical course of AD varies significantly among patients—from very mild itching and skin rash to severe cases of skin infection requiring intensive treatment. While the condition is usually seen in early childhood, AD can present initially in adulthood. Typically, the rash has a symmetrical distribution, concentrating in the flexural folds of the arms, backs of the legs, and neck. AD is considered a result of a complex relationship between genetics, environment, immune system dysregulation and skin barrier dysfunction.
AD symptoms often disrupt quality of life by affecting sleep and self-esteem, as well as school and work attendance. Although AD is not a curable disease, it usually can be successfully managed by a combination of skin care, avoidance of triggers, infection control, stress management and medical treatment.
Atopic dermatitis (AD), often termed “eczema”, is a chronic pruritic skin condition that affects about 10-20% of children and about 2-3% of adults. It is characterized by extreme itching, dry skin, scaling, erythematous papules, excoriations and exudates. These symptoms may be associated with frequent skin infections, as well as an increased incidence of allergic rhinitis, food allergy, and asthma.
The clinical course of AD varies significantly among patients—from very mild itching and skin rash to severe cases of skin infection requiring intensive treatment. While the condition is usually seen in early childhood, AD can present initially in adulthood. Typically, the rash has a symmetrical distribution, concentrating in the flexural folds of the arms, backs of the legs, and neck. AD is considered a result of a complex relationship between genetics, environment, immune system dysregulation and skin barrier dysfunction.
AD symptoms often disrupt quality of life by affecting sleep and self-esteem, as well as school and work attendance. Although AD is not a curable disease, it usually can be successfully managed by a combination of skin care, avoidance of triggers, infection control, stress management and medical treatment.
Genetics
Genetics greatly affect the risk of developing AD. For example: in a set of twins, when one twin has AD, the likelihood of the second twin developing AD is several times greater than that of the general population. While this illustrates the genetic nature of AD, there is no simple inheritance pattern to explain the disease. Instead, AD is thought to be the result of multiple genetic polymorphisms.
Loss-of-function mutations of the epidermal barrier protein filaggrin predispose a subset of patients to developing AD.
Other gene loci may be impaired in AD. These genes control T helper cell cytokine genes such as IL-4, IL-5 and IL-13. These cytokines are overproduced in atopic individuals and are linked to the IgE response to allergens as well as eosinophilia. There is a high concordance rate of AD among both fraternal and identical twins, indicating a definite role of genetics in development of the disease.
Genetics greatly affect the risk of developing AD. For example: in a set of twins, when one twin has AD, the likelihood of the second twin developing AD is several times greater than that of the general population. While this illustrates the genetic nature of AD, there is no simple inheritance pattern to explain the disease. Instead, AD is thought to be the result of multiple genetic polymorphisms.
Loss-of-function mutations of the epidermal barrier protein filaggrin predispose a subset of patients to developing AD.
Other gene loci may be impaired in AD. These genes control T helper cell cytokine genes such as IL-4, IL-5 and IL-13. These cytokines are overproduced in atopic individuals and are linked to the IgE response to allergens as well as eosinophilia. There is a high concordance rate of AD among both fraternal and identical twins, indicating a definite role of genetics in development of the disease.
Natural history
Although worldwide prevalence of AD varies, the occurrence in U.S. school children is roughly 17%. AD can be mild (80% of cases), moderate (18% of cases), or severe (2% of cases). In about 80% of affected children, the disease presents prior to their fifth birthday. More than 60% of AD-affected children experience resolution by adolescence. Further, more than 60% of AD-affected children are at risk for developing either respiratory allergy or asthma. In those patients with more severe disease in childhood, it is more likely to persist into adulthood.
Although worldwide prevalence of AD varies, the occurrence in U.S. school children is roughly 17%. AD can be mild (80% of cases), moderate (18% of cases), or severe (2% of cases). In about 80% of affected children, the disease presents prior to their fifth birthday. More than 60% of AD-affected children experience resolution by adolescence. Further, more than 60% of AD-affected children are at risk for developing either respiratory allergy or asthma. In those patients with more severe disease in childhood, it is more likely to persist into adulthood.
Increased incidence of allergy
AD is related to the development of food allergies, allergic rhinitis and asthma. In most patients with AD, there is an increased production of IgE in response to environmental allergens and food proteins. In fact, the total IgE level can be very high in active AD, often exceeding that seen in common respiratory allergy.
Allergen-specific IgE binds to mast cells in the skin. Upon exposure to allergens, mast cells degranulate and release inflammatory mediators leading to itching. Acute skin lesions in patients with AD show an increased level of TH2 (helper) cells expressing Il-4, IL-5 and IL-13 mRNA. These cytokines are secreted as part of the classic allergic response. In addition, skin scratching causes skin injury, activating keratinocytes to release further cytokines. This induces the expression of adhesion molecules on vascular endothelium and facilitates movement of inflammatory cells into the tissue.
AD is related to the development of food allergies, allergic rhinitis and asthma. In most patients with AD, there is an increased production of IgE in response to environmental allergens and food proteins. In fact, the total IgE level can be very high in active AD, often exceeding that seen in common respiratory allergy.
Allergen-specific IgE binds to mast cells in the skin. Upon exposure to allergens, mast cells degranulate and release inflammatory mediators leading to itching. Acute skin lesions in patients with AD show an increased level of TH2 (helper) cells expressing Il-4, IL-5 and IL-13 mRNA. These cytokines are secreted as part of the classic allergic response. In addition, skin scratching causes skin injury, activating keratinocytes to release further cytokines. This induces the expression of adhesion molecules on vascular endothelium and facilitates movement of inflammatory cells into the tissue.
Role of the skin as a barrier
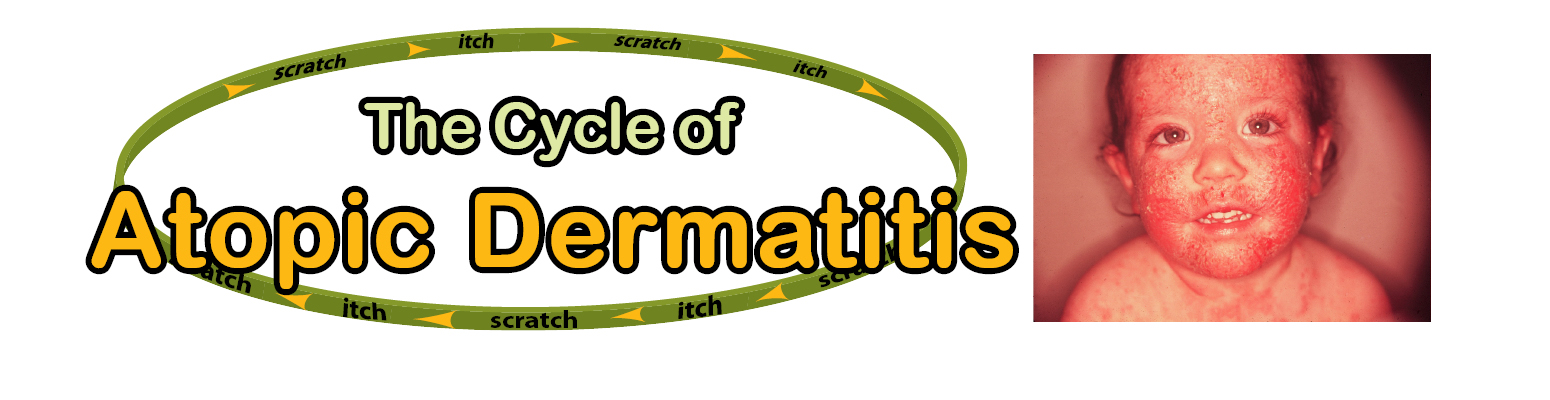
Does the rash cause the itching and scratching? Or does the itching and scratching cause the rash? It is unclear which comes first. It is known that the breakdown of the skin barrier by scratching and irritants can cause an AD flare. Further, the resulting pro-inflammatory cascade occurring within the skin can induce a patient to scratch more, further damaging the skin. This sequence evolves into an itch-scratch-itch cycle.
In normal skin, the stratum corneum of the epidermis is made up of dermosomes linking keratinocytes together. A lipid matrix made up of cholesterol, ceramides and fatty acids is crucial in protecting the skin barrier as well. AD is associated with breakdown of this barrier, including reduced ceramide levels, increased transepidermal water loss and increased activity of endogenous proteolytic enzymes. This barrier can be further weakened by exogenous proteases (e.g. dust mite allergens or exotoxins from Staph aureus bacteria). Therefore, dust mites and staph aureus are two potential triggers of AD.
Does the rash cause the itching and scratching? Or does the itching and scratching cause the rash? It is unclear which comes first. It is known that the breakdown of the skin barrier by scratching and irritants can cause an AD flare. Further, the resulting pro-inflammatory cascade occurring within the skin can induce a patient to scratch more, further damaging the skin. This sequence evolves into an itch-scratch-itch cycle.
In normal skin, the stratum corneum of the epidermis is made up of dermosomes linking keratinocytes together. A lipid matrix made up of cholesterol, ceramides and fatty acids is crucial in protecting the skin barrier as well. AD is associated with breakdown of this barrier, including reduced ceramide levels, increased transepidermal water loss and increased activity of endogenous proteolytic enzymes. This barrier can be further weakened by exogenous proteases (e.g. dust mite allergens or exotoxins from Staph aureus bacteria). Therefore, dust mites and staph aureus are two potential triggers of AD.
Clinical features
The diagnosis of AD is based on the presence of major and minor features (see Table 1).
Acute AD is characterized by intensely pruritic, erythematous papules associated with excoriations, vesiculations, and serous exudate. Subacute AD is characterized by erythematous, excoriated, scaling papules. Chronic AD is characterized by thickened skin (lichenification) with accentuated markings and changes in pigmentation and fibrotic papules. Patients with chronic AD may have all three types of lesions simultaneously. In addition, patients usually complain of dry skin.
During infancy, AD primarily affects the face, the scalp, and the extensor surfaces of the extremities. The diaper area is usually spared, but if involved, it may be secondarily infected with Candida, in which case the dermatitis does not spare the inguinal folds. In contrast, lower extremity involvement is a common distribution in children. In older patients with long-standing disease, the flexural folds of the extremities are the predominant location of lesions (popliteal fossa and antecubital fossa). Localized AD involving the eyelids and periocular skin more often affects adults and may be an isolated manifestation, but it should be differentiated from allergic contact dermatitis.
The diagnosis of AD is based on the presence of major and minor features (see Table 1).
Acute AD is characterized by intensely pruritic, erythematous papules associated with excoriations, vesiculations, and serous exudate. Subacute AD is characterized by erythematous, excoriated, scaling papules. Chronic AD is characterized by thickened skin (lichenification) with accentuated markings and changes in pigmentation and fibrotic papules. Patients with chronic AD may have all three types of lesions simultaneously. In addition, patients usually complain of dry skin.
During infancy, AD primarily affects the face, the scalp, and the extensor surfaces of the extremities. The diaper area is usually spared, but if involved, it may be secondarily infected with Candida, in which case the dermatitis does not spare the inguinal folds. In contrast, lower extremity involvement is a common distribution in children. In older patients with long-standing disease, the flexural folds of the extremities are the predominant location of lesions (popliteal fossa and antecubital fossa). Localized AD involving the eyelids and periocular skin more often affects adults and may be an isolated manifestation, but it should be differentiated from allergic contact dermatitis.
Ocular complications of AD
Atopic keratoconjunctivitis is almost always bilateral, and symptoms include itching, burning, tearing, and mucoid discharge. It is frequently associated with eyelid dermatitis and chronic blepharitis and may result in visual impairment from corneal scarring. Keratoconus is a conical deformity of the cornea that is believed to result from persistent rubbing of the eyes in patients with AD and allergic rhinitis. Anterior subcapsular cataracts may develop during adolescence or early adult life as a complication of AD.
Atopic keratoconjunctivitis is almost always bilateral, and symptoms include itching, burning, tearing, and mucoid discharge. It is frequently associated with eyelid dermatitis and chronic blepharitis and may result in visual impairment from corneal scarring. Keratoconus is a conical deformity of the cornea that is believed to result from persistent rubbing of the eyes in patients with AD and allergic rhinitis. Anterior subcapsular cataracts may develop during adolescence or early adult life as a complication of AD.
Hand dermatitis complicating AD
Patients with AD often have non-specific hand dermatitis. This is frequently irritant in nature and aggravated by repeated wetting or washing, especially in the occupational setting. A history of past or present AD at least doubles the effects of irritant exposure and doubles the risk in occupations where hand eczema is a common problem.
Patients with AD often have non-specific hand dermatitis. This is frequently irritant in nature and aggravated by repeated wetting or washing, especially in the occupational setting. A history of past or present AD at least doubles the effects of irritant exposure and doubles the risk in occupations where hand eczema is a common problem.
Skin infections complicating AD
Patients with AD have an increased susceptibility to infection or colonization with a variety of organisms. These include viral infections with herpes simplex, molluscum contagiosum, and human papillomavirus. A direct relationship has been demonstrated between interferon-γ (IFN-γ) concentrations and the cytopathic effect of herpes simplex. Also, an inverse relationship has been established between IL-4 and the cytopathic effect of herpes simplex, suggesting that the T cell-associated cytokine abnormalities seen in AD can enhance the effect of viral infections, like herpes.
A number of studies have noted the importance of Staphylococcus aureus in AD. The higher rate of S. aureus colonization in AD lesions compared to lesions from other skin disorders may also be associated with staph colonization of the nares, with the hands serving as the vector of transmission.
Patients without obvious superinfection may have a better response to combined antistaphylococcal and topical corticosteroid therapy than to corticosteroids alone. Although recurrent staphylococcal pustulosis can be a significant problem in AD, invasive S. aureus infections occur rarely and should raise the possibility of an immunodeficiency such as hyper-IgE syndrome. Chronic skin inflammatory lesions in AD reveal dry, thickened, lichenified (leather-like) skin that is often hyper or hypo- pigmented. AD usually follows a chronic relapsing course which may flare due to allergens, changes in temperature and/or humidity, and stress.
Patients with AD have an increased susceptibility to infection or colonization with a variety of organisms. These include viral infections with herpes simplex, molluscum contagiosum, and human papillomavirus. A direct relationship has been demonstrated between interferon-γ (IFN-γ) concentrations and the cytopathic effect of herpes simplex. Also, an inverse relationship has been established between IL-4 and the cytopathic effect of herpes simplex, suggesting that the T cell-associated cytokine abnormalities seen in AD can enhance the effect of viral infections, like herpes.
A number of studies have noted the importance of Staphylococcus aureus in AD. The higher rate of S. aureus colonization in AD lesions compared to lesions from other skin disorders may also be associated with staph colonization of the nares, with the hands serving as the vector of transmission.
Patients without obvious superinfection may have a better response to combined antistaphylococcal and topical corticosteroid therapy than to corticosteroids alone. Although recurrent staphylococcal pustulosis can be a significant problem in AD, invasive S. aureus infections occur rarely and should raise the possibility of an immunodeficiency such as hyper-IgE syndrome. Chronic skin inflammatory lesions in AD reveal dry, thickened, lichenified (leather-like) skin that is often hyper or hypo- pigmented. AD usually follows a chronic relapsing course which may flare due to allergens, changes in temperature and/or humidity, and stress.
Psychosocial implications of AD
Patients with AD may have higher levels of anxiety and problems dealing with anger, hostility and frustration. Although these emotions do not cause AD, they can exacerbate the illness. Patients often respond to stress or frustration by itching and scratching. Stimulation of the central nervous system may intensify cutaneous vasomotor and sweat responses and contribute to the itch–scratch cycle. In some instances, scratching is associated with significant secondary gain or may be a strong component of habit. Severe disease can have a significant impact on patients, leading to problems with social interactions and self-esteem. Of considerable importance, sleep disturbance due to itching is common in this chronic disease and significantly impacts on the quality of life of patients and family members.
Patients with AD may have higher levels of anxiety and problems dealing with anger, hostility and frustration. Although these emotions do not cause AD, they can exacerbate the illness. Patients often respond to stress or frustration by itching and scratching. Stimulation of the central nervous system may intensify cutaneous vasomotor and sweat responses and contribute to the itch–scratch cycle. In some instances, scratching is associated with significant secondary gain or may be a strong component of habit. Severe disease can have a significant impact on patients, leading to problems with social interactions and self-esteem. Of considerable importance, sleep disturbance due to itching is common in this chronic disease and significantly impacts on the quality of life of patients and family members.
Treatment
The treatment of AD must be optimized for each patient, taking into consideration the role of environment, allergens, irritants, response to medication, and psychosocial stresses in the disease process. Patients and/or their families must also be counseled that AD is a chronic disease that cannot be cured but can usually be successfully managed with proper daily care.
The treatment of AD must be optimized for each patient, taking into consideration the role of environment, allergens, irritants, response to medication, and psychosocial stresses in the disease process. Patients and/or their families must also be counseled that AD is a chronic disease that cannot be cured but can usually be successfully managed with proper daily care.
1.Eliminate exacerbating factors
Patients with AD have a lower tolerance to environmental irritants, which include: detergents, soaps, chemicals, pollutants, abrasives, extreme temperatures and humidity. All cleansers and detergents should be fragrance- and irritant-free. Soaps with minimal defatting activity and neutral pH should be used (e.g., Dove, Neutrogena, Cetaphil).
Clothes should be rinsed twice in the wash, without fabric softener that may irritate the skin. All new clothing should be washed before wearing to remove chemicals. Some irritating fabrics such as wool should be avoided altogether. Air conditioning should be used in the summer. Hot, humid weather and sweating can flare AD. In the winter, judicious use of a humidifier can help with dry, itchy skin. Occlusive clothing should be avoided, and cotton or cotton blends are recommended. The temperature in the home and work environments should be temperate to minimize sweating.
Other irritants may include chlorine or bromine in swimming pools, although swimming and sun exposure themselves may be beneficial for AD patients.
Patients with AD have a lower tolerance to environmental irritants, which include: detergents, soaps, chemicals, pollutants, abrasives, extreme temperatures and humidity. All cleansers and detergents should be fragrance- and irritant-free. Soaps with minimal defatting activity and neutral pH should be used (e.g., Dove, Neutrogena, Cetaphil).
Clothes should be rinsed twice in the wash, without fabric softener that may irritate the skin. All new clothing should be washed before wearing to remove chemicals. Some irritating fabrics such as wool should be avoided altogether. Air conditioning should be used in the summer. Hot, humid weather and sweating can flare AD. In the winter, judicious use of a humidifier can help with dry, itchy skin. Occlusive clothing should be avoided, and cotton or cotton blends are recommended. The temperature in the home and work environments should be temperate to minimize sweating.
Other irritants may include chlorine or bromine in swimming pools, although swimming and sun exposure themselves may be beneficial for AD patients.
n Allergens / irritants
Allergy skin testing or RAST/Immunocap™ assay is valuable in the identification of environmental and food allergies contributing to AD. Specific IgE measurement using a lab assay can also assess sensitivity to certain foods such as eggs, milk, peanuts and fish. There is some proof that reducing dust mite exposure in dust-allergic patients may improve AD. This includes using dust mite encasements on mattresses and pillows, removing carpets and washing linens in very hot water.
Positive allergy skin tests are considered relevant when they correlate with the patient’s allergy history. This is an important point since some patients with AD produce large amounts of specific IgE that does not appear clinically relevant.
Allergy skin testing or RAST/Immunocap™ assay is valuable in the identification of environmental and food allergies contributing to AD. Specific IgE measurement using a lab assay can also assess sensitivity to certain foods such as eggs, milk, peanuts and fish. There is some proof that reducing dust mite exposure in dust-allergic patients may improve AD. This includes using dust mite encasements on mattresses and pillows, removing carpets and washing linens in very hot water.
Positive allergy skin tests are considered relevant when they correlate with the patient’s allergy history. This is an important point since some patients with AD produce large amounts of specific IgE that does not appear clinically relevant.
n Hydration / moisturizers
Daily skin care and moisturizing is imperative when treating AD. Improving skin hydration helps to restore skin barrier function. Daily baths in warm water lasting 10-20 minutes followed by immediate application of an effective emollient cream or ointment to lock in moisture are recommended. Some patients may use oatmeal baths to soothe the skin. Moisturizers should be scent- and irritant-free. Ointments are generally preferred, as they tend to have fewer preservatives. Crisco shortening can even be used as an inexpensive moisturizer. Newer barrier creams have been developed that help repair the skin barrier (e.g., Atopiclair, Epicream, and Mimyx). These newer barrier creams can help restore the integrity of the dry skin in AD and offer great benefit to many patients. All of these newer barrier creams require a prescription.
Wet wrap dressings at bedtime can be used in cases of severe flares of AD by decreasing the itch and inflammation. The wet bandages are placed over a dilute corticosteroid preparation on the skin. The area is then over-wrapped with a dry bandage. This can be done for several nights. When the skin is inflamed and covered with pus, gently use wet dressings to remove pus and bacteria prior to applying therapy to the underlying inflamed skin (see antibiotic treatment below).
Daily skin care and moisturizing is imperative when treating AD. Improving skin hydration helps to restore skin barrier function. Daily baths in warm water lasting 10-20 minutes followed by immediate application of an effective emollient cream or ointment to lock in moisture are recommended. Some patients may use oatmeal baths to soothe the skin. Moisturizers should be scent- and irritant-free. Ointments are generally preferred, as they tend to have fewer preservatives. Crisco shortening can even be used as an inexpensive moisturizer. Newer barrier creams have been developed that help repair the skin barrier (e.g., Atopiclair, Epicream, and Mimyx). These newer barrier creams can help restore the integrity of the dry skin in AD and offer great benefit to many patients. All of these newer barrier creams require a prescription.
Wet wrap dressings at bedtime can be used in cases of severe flares of AD by decreasing the itch and inflammation. The wet bandages are placed over a dilute corticosteroid preparation on the skin. The area is then over-wrapped with a dry bandage. This can be done for several nights. When the skin is inflamed and covered with pus, gently use wet dressings to remove pus and bacteria prior to applying therapy to the underlying inflamed skin (see antibiotic treatment below).
n Everyday skin care for AD
A simple and basic regimen is key to effective AD management. Staying with one well-tolerated soap and one moisturizer is very important. Using multiple soaps, lotions, fragrances, and mixes of products may cause further irritation of sensitive skin.
Maintaining the skin barrier will prevent further damage and enhance the patient’s quality of life. An effective daily skin care routine is critical in preventing recurrent episodes of symptoms. Key factors are proper bathing and the application of lubricants, such as creams or ointments. People with atopic dermatitis should avoid hot or long baths and showers (more than 20 minutes). A warm bath helps to cleanse and moisturize the skin without drying it excessively. The doctor may recommend limited use of a mild soap or non-soap cleanser (Cetaphil) because soaps can be drying to the skin. Bath oils are not usually helpful.
Once the bath is finished (10-20 minutes), the patient should air-dry the skin or pat it dry gently with a soft towel (avoiding rubbing or brisk drying) and apply a lubricant immediately. Lubrication locks in the skin’s moisture acquired from bathing, increases the rate of healing, and establishes a barrier against further drying and irritation. Several kinds of lubricants can be used. Lotions are generally not the best choice because they have a high water or alcohol content and evaporate quickly. Creams and ointments work better in healing the skin. Tar preparations can be very helpful in healing dry thickened, lichenified areas. The chosen preparation should be as free of fragrances and chemicals as possible.
Another key to protecting and restoring the skin is taking steps to avoid repeated skin infections. Although it may not be possible to avoid infections altogether, early identification and treatment is best.
A simple and basic regimen is key to effective AD management. Staying with one well-tolerated soap and one moisturizer is very important. Using multiple soaps, lotions, fragrances, and mixes of products may cause further irritation of sensitive skin.
Maintaining the skin barrier will prevent further damage and enhance the patient’s quality of life. An effective daily skin care routine is critical in preventing recurrent episodes of symptoms. Key factors are proper bathing and the application of lubricants, such as creams or ointments. People with atopic dermatitis should avoid hot or long baths and showers (more than 20 minutes). A warm bath helps to cleanse and moisturize the skin without drying it excessively. The doctor may recommend limited use of a mild soap or non-soap cleanser (Cetaphil) because soaps can be drying to the skin. Bath oils are not usually helpful.
Once the bath is finished (10-20 minutes), the patient should air-dry the skin or pat it dry gently with a soft towel (avoiding rubbing or brisk drying) and apply a lubricant immediately. Lubrication locks in the skin’s moisture acquired from bathing, increases the rate of healing, and establishes a barrier against further drying and irritation. Several kinds of lubricants can be used. Lotions are generally not the best choice because they have a high water or alcohol content and evaporate quickly. Creams and ointments work better in healing the skin. Tar preparations can be very helpful in healing dry thickened, lichenified areas. The chosen preparation should be as free of fragrances and chemicals as possible.
Another key to protecting and restoring the skin is taking steps to avoid repeated skin infections. Although it may not be possible to avoid infections altogether, early identification and treatment is best.
n Corticosteroids
Topical corticosteroids remain the first line of active treatment for AD and when employed judiciously, their efficacy far outweighs any potential side effects. Topical steroid creams and ointments reduce both inflammation and pruritus. Corticosteroids vary in their potency (see Table 3). The vehicle used in the preparation can also alter the penetration and efficacy of the steroid. Rarely should steroids be used under occlusion as this may cause irreversible atrophic changes to the underlying skin.
In general, the use of medium to low potency steroids should not cause side effects if used properly. Side effects may include thinning of the skin, telangectasia, acne, stria, and hypo pigmentation. Particular care should be taken when treating areas such as the face, eye area and groin as these areas are more susceptible to adverse side effects. In rare cases, patients can develop contact allergy to the steroid creams or their preservatives.
Steroids can come in many forms including lotions, creams, ointments, oils, foams and even tapes. Ointments are more occlusive and have longer staying power, but they are often too greasy for daily use. Foams are good for the scalp and beard area but may contain alcohol, which is drying. It is important not to abruptly discontinue topical therapy with a high potency corticosteroid, as this may cause a flare of AD. One should institute step therapy in AD moving from high potency to a low potency therapy to avoid flares of AD. In general, oral prednisone should be used sparingly to manage AD, as its taper may be associated with a dramatic flare of AD symptoms.
In contrast, undertreating AD may cause sleep loss, decreased work or school productivity, skin wounds, infection, and possibly psychosocial pathology.
Topical corticosteroids remain the first line of active treatment for AD and when employed judiciously, their efficacy far outweighs any potential side effects. Topical steroid creams and ointments reduce both inflammation and pruritus. Corticosteroids vary in their potency (see Table 3). The vehicle used in the preparation can also alter the penetration and efficacy of the steroid. Rarely should steroids be used under occlusion as this may cause irreversible atrophic changes to the underlying skin.
In general, the use of medium to low potency steroids should not cause side effects if used properly. Side effects may include thinning of the skin, telangectasia, acne, stria, and hypo pigmentation. Particular care should be taken when treating areas such as the face, eye area and groin as these areas are more susceptible to adverse side effects. In rare cases, patients can develop contact allergy to the steroid creams or their preservatives.
Steroids can come in many forms including lotions, creams, ointments, oils, foams and even tapes. Ointments are more occlusive and have longer staying power, but they are often too greasy for daily use. Foams are good for the scalp and beard area but may contain alcohol, which is drying. It is important not to abruptly discontinue topical therapy with a high potency corticosteroid, as this may cause a flare of AD. One should institute step therapy in AD moving from high potency to a low potency therapy to avoid flares of AD. In general, oral prednisone should be used sparingly to manage AD, as its taper may be associated with a dramatic flare of AD symptoms.
In contrast, undertreating AD may cause sleep loss, decreased work or school productivity, skin wounds, infection, and possibly psychosocial pathology.
n Topical calcineurin inhibitors (TCIs)
TCIs are nonsteroidal immunomodulating drugs that block the inflammatory cascade produced by T-cells in the skin. There are two TCIs available in the U.S.: tacrolimus 0.03% and 0.1% ointment (Protopic) and Pimecrolimus 1% cream (Elidel). They are indicated for treatment of moderate to severe AD in non-immunocompromised adults and children older than two years. TCIs may cause transient burning when first applied. Since they do not cause skin atrophy, they can be used in the groin and on the face. TCIs have demonstrated low systemic absorption as compared to corticosteroids. Despite their inherent safety, TCIs carry a black box warning stating that “long-term safety has not been established.” As an immunosuppressive drug, there is a theoretical increased risk of malignancy.
TCIs are nonsteroidal immunomodulating drugs that block the inflammatory cascade produced by T-cells in the skin. There are two TCIs available in the U.S.: tacrolimus 0.03% and 0.1% ointment (Protopic) and Pimecrolimus 1% cream (Elidel). They are indicated for treatment of moderate to severe AD in non-immunocompromised adults and children older than two years. TCIs may cause transient burning when first applied. Since they do not cause skin atrophy, they can be used in the groin and on the face. TCIs have demonstrated low systemic absorption as compared to corticosteroids. Despite their inherent safety, TCIs carry a black box warning stating that “long-term safety has not been established.” As an immunosuppressive drug, there is a theoretical increased risk of malignancy.
n Tar preparations
Although not as commonly used, crude coal tar extracts have mild anti-inflammatory properties that may help limit the use of corticosteroids. They are especially helpful on the scalp in shampoo form. The side effects are minimal and generally are limited to skin irritation, strong odor, photosensitivity and pustular folliculitis.
Although not as commonly used, crude coal tar extracts have mild anti-inflammatory properties that may help limit the use of corticosteroids. They are especially helpful on the scalp in shampoo form. The side effects are minimal and generally are limited to skin irritation, strong odor, photosensitivity and pustular folliculitis.
n Antibiotics
It is not uncommon for secondary infection to occur in AD, and it is often due to Staphylococcus aureus. Most patients with AD have higher levels of colonization with S. aureus. S. aureus secretes an exotoxin that causes local skin destruction and intense itching. In flares of AD when pustules are seen, short courses of either a semi-synthetic penicillin or a first- or second-generation cephalosporin for 7-10 days is usually effective. Chlorine or dilute bleach baths may also be helpful.
It is not uncommon for secondary infection to occur in AD, and it is often due to Staphylococcus aureus. Most patients with AD have higher levels of colonization with S. aureus. S. aureus secretes an exotoxin that causes local skin destruction and intense itching. In flares of AD when pustules are seen, short courses of either a semi-synthetic penicillin or a first- or second-generation cephalosporin for 7-10 days is usually effective. Chlorine or dilute bleach baths may also be helpful.
n Antipruritic agents
Itching is the hallmark of AD and causes the most suffering in patients. In fact, from a diagnostic point of view, a rash without itching rules out atopic dermatitis as a diagnostic consideration. Typical antipruritic drugs such as antihistamines may not be completely effective in controlling AD itching because it is likely caused by cytokines or neuropeptides rather than histamine release alone. Most of the benefits of using antihistamines in AD patients may stem from their sedating and tranquilizing effects. Diphenhydramine, because of its quick onset and short half-life may benefit children while tricylic antidepressants such as doxepin may be helpful in treating adults. Use of topical antihistamines or topical anesthetics has been shown to cause sensitization in some patients and should be avoided.
Itching is the hallmark of AD and causes the most suffering in patients. In fact, from a diagnostic point of view, a rash without itching rules out atopic dermatitis as a diagnostic consideration. Typical antipruritic drugs such as antihistamines may not be completely effective in controlling AD itching because it is likely caused by cytokines or neuropeptides rather than histamine release alone. Most of the benefits of using antihistamines in AD patients may stem from their sedating and tranquilizing effects. Diphenhydramine, because of its quick onset and short half-life may benefit children while tricylic antidepressants such as doxepin may be helpful in treating adults. Use of topical antihistamines or topical anesthetics has been shown to cause sensitization in some patients and should be avoided.
n Allergen Immunotherapy
Allergen immunotherapy has shown some promising initial results in the treatment of AD. The most convincing benefits in these studies were found in house dust mite-sensitized AD patients. The potential side effects of allergen immunotherapy (including anaphylaxis and worsening of AD) need to be considered. Further studies are needed to compare this therapy with conventional AD treatment before it is considered a viable option.
Allergen immunotherapy has shown some promising initial results in the treatment of AD. The most convincing benefits in these studies were found in house dust mite-sensitized AD patients. The potential side effects of allergen immunotherapy (including anaphylaxis and worsening of AD) need to be considered. Further studies are needed to compare this therapy with conventional AD treatment before it is considered a viable option.
2. Patient education
AD can be an extremely disruptive chronic condition that interferes with sleep, work and school. Relaxation techniques, biofeedback, massage therapy and even psychotherapy may be helpful. The patient must be educated regarding triggers of AD, as well as the chronic nature of this condition.
AD can be an extremely disruptive chronic condition that interferes with sleep, work and school. Relaxation techniques, biofeedback, massage therapy and even psychotherapy may be helpful. The patient must be educated regarding triggers of AD, as well as the chronic nature of this condition.
3.Pruritus and sleep
Severe itching can seriously interfere with sleep. Use of first-generation antihistamines (diphenhydramine, and hydroxyzine) at bedtime may be a good idea since they often have a sedative effect. Doxepin, benzodiazepines, and clonidine have been used at bedtime in AD-affected adults as sleep aids, although they are not specifically approved for this purpose.
Severe itching can seriously interfere with sleep. Use of first-generation antihistamines (diphenhydramine, and hydroxyzine) at bedtime may be a good idea since they often have a sedative effect. Doxepin, benzodiazepines, and clonidine have been used at bedtime in AD-affected adults as sleep aids, although they are not specifically approved for this purpose.
4. Food allergy and AD
Nearly half of the children with moderate to severe AD suffer from some form of food allergy. The onset of reactions to foods may be immediate or delayed and may be associated with hives, itching and flares of AD, GI symptoms, or respiratory symptoms. Milk, soy, eggs, wheat, peanuts, shellfish, and tree nuts are the allergens that produce 90% of food allergy reactions.
Negative allergy skin testing for foods is 95% accurate. However, false positive tests are not uncommon and require a carefully monitored challenge to confirm the actual presence of food allergy. A history of food allergy triggering AD may be misleading. It should be supported by elimination of the suspected food and subsequent improvement of AD symptoms.
Nearly half of the children with moderate to severe AD suffer from some form of food allergy. The onset of reactions to foods may be immediate or delayed and may be associated with hives, itching and flares of AD, GI symptoms, or respiratory symptoms. Milk, soy, eggs, wheat, peanuts, shellfish, and tree nuts are the allergens that produce 90% of food allergy reactions.
Negative allergy skin testing for foods is 95% accurate. However, false positive tests are not uncommon and require a carefully monitored challenge to confirm the actual presence of food allergy. A history of food allergy triggering AD may be misleading. It should be supported by elimination of the suspected food and subsequent improvement of AD symptoms.
5. Skin infections and AD
It is common for secondary skin infections to occur in AD. These infections are often due to S. aureus. Most patients with AD have high levels of colonization. S. aureus secretes an exotoxin that causes local skin destruction and intense itching. In flares of AD when pustules are seen, short courses of either semi-synthetic penicillins or first or second-generation cephalosporins for 7-10 days are usually effective. For local areas of infection topical muropiricin (Bactroban) applied three times a day may also be effective. Treating nasal colonization of staph with nasal muropiricin twice a day for 5 days also may reduce flares of AD.
Although use of an antibacterial soap may decrease staph colonization of the skin, these soaps are often too drying and irritating. Instead, a mild lotion soap is preferred.
Another option is using bleach baths to decrease the incidence of skin infections. In this case, 1/8 cup of sodium hypoclorite (bleach) per full tub of water for a 10-15 minute soak several times a week may significantly reduce bacterial load and reduce flares in patients with persistent skin colonization.
In infants with extensive secondary skin infections or patients with persistent fevers, further work-up for more invasive infections (e.g., bacteremia, endocarditis, arthritis, osteomyelitis, bursitis) should be considered. Hospital admission for intravenous antibiotics and intensive nursing may be necessary.
Herpes simplex virus (HSV) can cause life-threatening eczema herpeticum in AD patients because of distinct susceptibility to this type of viral infection. Patients with eczema herpeticum may present with fever, malaise, and widespread vesicles. However, some HSV-superinfected AD lesions may not appear vesicular, but rather as punched-out lesions with an erythematous base. HSV DNA polymerase chain reaction (PCR), Tzanck smear, or viral culture should be obtained from the lesion while the patient is started on intravenous acyclovir or other antiviral medication. Patients with periocular or ocular involvement should be evaluated by an ophthalmologist as an emergency. Since smallpox vaccine is no longer available, the resulting life threatening infection of eczema vaccinatum is no longer encountered.
It is common for secondary skin infections to occur in AD. These infections are often due to S. aureus. Most patients with AD have high levels of colonization. S. aureus secretes an exotoxin that causes local skin destruction and intense itching. In flares of AD when pustules are seen, short courses of either semi-synthetic penicillins or first or second-generation cephalosporins for 7-10 days are usually effective. For local areas of infection topical muropiricin (Bactroban) applied three times a day may also be effective. Treating nasal colonization of staph with nasal muropiricin twice a day for 5 days also may reduce flares of AD.
Although use of an antibacterial soap may decrease staph colonization of the skin, these soaps are often too drying and irritating. Instead, a mild lotion soap is preferred.
Another option is using bleach baths to decrease the incidence of skin infections. In this case, 1/8 cup of sodium hypoclorite (bleach) per full tub of water for a 10-15 minute soak several times a week may significantly reduce bacterial load and reduce flares in patients with persistent skin colonization.
In infants with extensive secondary skin infections or patients with persistent fevers, further work-up for more invasive infections (e.g., bacteremia, endocarditis, arthritis, osteomyelitis, bursitis) should be considered. Hospital admission for intravenous antibiotics and intensive nursing may be necessary.
Herpes simplex virus (HSV) can cause life-threatening eczema herpeticum in AD patients because of distinct susceptibility to this type of viral infection. Patients with eczema herpeticum may present with fever, malaise, and widespread vesicles. However, some HSV-superinfected AD lesions may not appear vesicular, but rather as punched-out lesions with an erythematous base. HSV DNA polymerase chain reaction (PCR), Tzanck smear, or viral culture should be obtained from the lesion while the patient is started on intravenous acyclovir or other antiviral medication. Patients with periocular or ocular involvement should be evaluated by an ophthalmologist as an emergency. Since smallpox vaccine is no longer available, the resulting life threatening infection of eczema vaccinatum is no longer encountered.
Stubborn AD
Hospitalization
In rare cases of severe atopic dermatitis that are resistant to therapy or in patients with disseminated infection, short-term hospital stays may be necessary. Merely removing the patient from his/her environment and ensuring compliance with intensive skin care may result in marked clinical improvement.
Hospitalization
In rare cases of severe atopic dermatitis that are resistant to therapy or in patients with disseminated infection, short-term hospital stays may be necessary. Merely removing the patient from his/her environment and ensuring compliance with intensive skin care may result in marked clinical improvement.
a. Systemic corticosteroids
This is an aggressive treatment for symptomatic relief of a severe AD flare. A short 1-week course of systemic corticosteroids should be followed by a taper over a few days and more intensive daily skin care (i.e., increase bathing frequency and the amount and type of topical corticosteroids), due to the potential of rebound AD symptoms when discontinuing systemic corticosteroids. The side effects of repeat or prolonged courses of systemic corticosteroids include adrenal suppression, growth retardation in children, osteoporosis, hypertension, peptic ulcer, glaucoma, cataracts, and infections due to immunosuppression.
This is an aggressive treatment for symptomatic relief of a severe AD flare. A short 1-week course of systemic corticosteroids should be followed by a taper over a few days and more intensive daily skin care (i.e., increase bathing frequency and the amount and type of topical corticosteroids), due to the potential of rebound AD symptoms when discontinuing systemic corticosteroids. The side effects of repeat or prolonged courses of systemic corticosteroids include adrenal suppression, growth retardation in children, osteoporosis, hypertension, peptic ulcer, glaucoma, cataracts, and infections due to immunosuppression.
b. Cyclosporin A
In severe AD, intermittent or continuous treatment with low-dose cyclosporin A (2.5-5 mg/kg/day) for up to one year showed significant improvements in disease activity as well as decreases in pruritus and sleep disturbances in clinical studies. Use of cyclosporin is limited due to possible nephrotoxicity and is reserved for severe AD cases.
In severe AD, intermittent or continuous treatment with low-dose cyclosporin A (2.5-5 mg/kg/day) for up to one year showed significant improvements in disease activity as well as decreases in pruritus and sleep disturbances in clinical studies. Use of cyclosporin is limited due to possible nephrotoxicity and is reserved for severe AD cases.
c. Phototherapy/PUVA UV light therapy can be a very effective modality for treating stubborn AD, especially in those patients who are not light skinned and do not flare after sun exposure. Phototherapy exerts its effect by decreasing the expression of activated T-cells. UVA therapy has been used under medical supervision. This therapy may decrease dermal IgE binding cells and down regulate pro-inflammatory cytokines. Similarly, photochemotherapy using oral methoxypsoralen therapy followed by UVA (PUVA) is indicated for severe cases. Short- and long-term side effects may include pruritus, erythema, pigmentation, premature aging, and cutaneous malignancies. Natural phototherapy may also benefit patients, and sun exposure at the Dead Sea has been touted as a natural treatment for skin diseases including AD.
d. Azathioprine
Azathioprine has been shown to be effective in managing several dermatologic diseases and can be used in severe AD not responsive to other therapies. It acts as a systemic immunosuppressive agent and has the risk of numerous side effects including myelosuppression, hepatotoxicity, GI disturbance and increased risk of infection. Patients must be screened prior to treatment for levels of the enzyme thiopurine methyl transferase (TPMT) and the dose adjusted based on this level. Treatment may take months before an effect is seen.
Azathioprine has been shown to be effective in managing several dermatologic diseases and can be used in severe AD not responsive to other therapies. It acts as a systemic immunosuppressive agent and has the risk of numerous side effects including myelosuppression, hepatotoxicity, GI disturbance and increased risk of infection. Patients must be screened prior to treatment for levels of the enzyme thiopurine methyl transferase (TPMT) and the dose adjusted based on this level. Treatment may take months before an effect is seen.
e. Other treatments
There are several other therapies that have been used to treat severe AD, however, their benefit has not been proven. Probiotics have not been proven to be effective for AD, nor has the efficacy of Chinese medicinal herbs. There is currently no convincing data to support the use of intravenous immunoglobulin (IVIG) or Omalizumab (Xolair) to treat AD. Double-blind, placebo-controlled trials have failed to show the efficacy of montelukast.
There are several other therapies that have been used to treat severe AD, however, their benefit has not been proven. Probiotics have not been proven to be effective for AD, nor has the efficacy of Chinese medicinal herbs. There is currently no convincing data to support the use of intravenous immunoglobulin (IVIG) or Omalizumab (Xolair) to treat AD. Double-blind, placebo-controlled trials have failed to show the efficacy of montelukast.
Conclusions
Atopic dermatitis is a common skin condition whose prevalence is on the rise among children and adults. As research continues to elucidate the many factors contributing to atopic dermatitis, we are better able to treat and manage the outcome. Crucial to management is identification of allergic triggers, daily skin care and intense patient education. Along with the excellent treatment options we have currently at our disposal, new insights into the origins and mechanisms behind AD should yield even better therapeutic alternatives in the future.